2025-09-21
Alzheimer’s in a drop of blood?
Neurology
By Ana Espino | Published on september 21, 2025 | 3 min read
#Alzheimer #Tau #Neurology
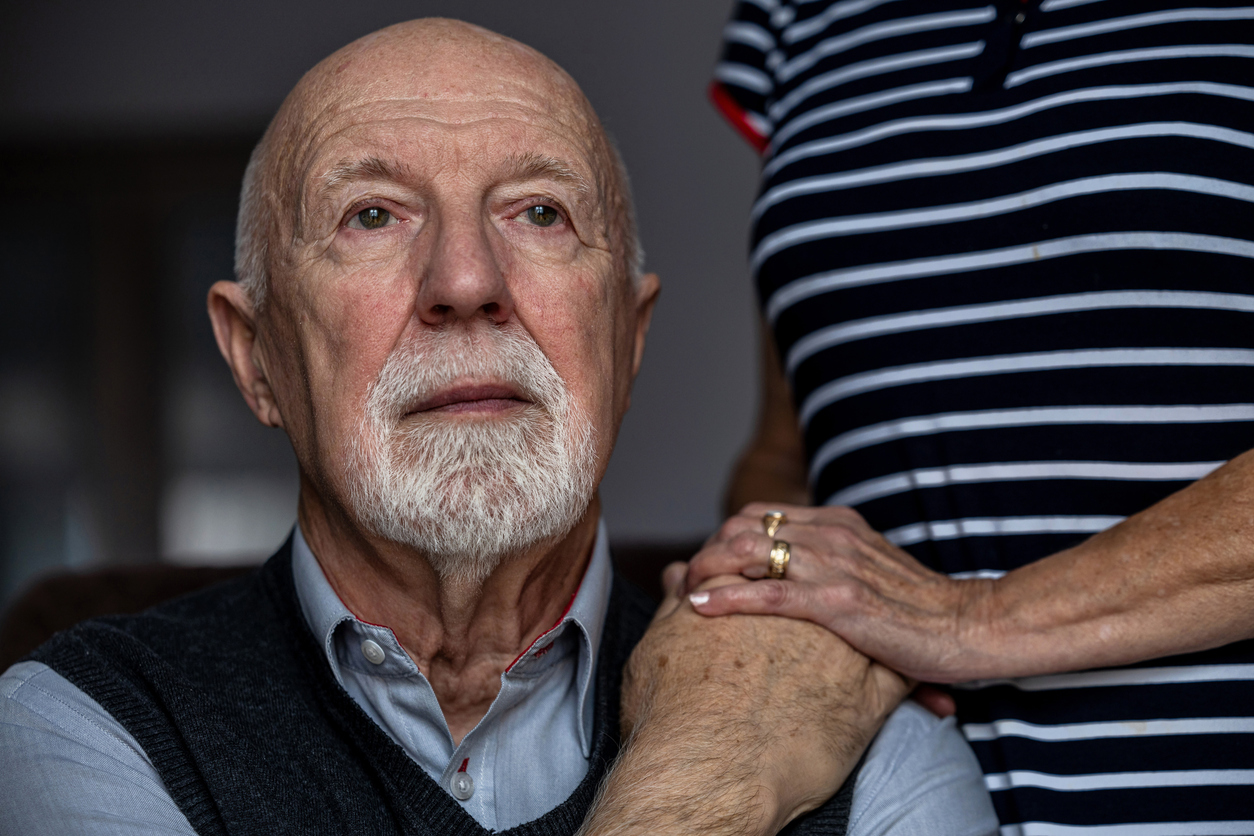
Alzheimer’s disease is a progressive neurodegenerative disorder, responsible for irreversible cognitive decline and loss of autonomy, associated with the abnormal accumulation of beta-amyloid and phosphorylated tau in the brain. It is the leading cause of dementia worldwide. Diagnosis still relies heavily on invasive and costly tools: cerebrospinal fluid (CSF) biomarkers, brain imaging (amyloid or tau PET), and complex clinical assessments, which are often difficult to access in everyday practice. These limitations hinder early screening and the implementation of targeted therapeutic strategies, particularly in the silent stages of the disease.
In this context, a major challenge lies in the identification and development of reliable peripheral biomarkers, capable of detecting Alzheimer’s from its earliest stages, distinguishing it from other causes of dementia, and being easily integrated into primary care.
This review was therefore conducted to explore the diagnostic potential of blood-based phosphorylated tau markers (p-tau181, p-tau217, p-tau231), by analyzing their accuracy, their correlation with central biomarkers, and their clinical applicability on a large scale.
This review is based on a critical analysis of longitudinal and cross-sectional clinical studies, conducted on cohorts of patients with Alzheimer’s, individuals with mild cognitive impairment (MCI), and healthy controls. Plasma concentrations of phosphorylated tau (p-tau181, p-tau217, p-tau231) were systematically compared with CSF biomarkers, amyloid and tau PET imaging, and clinical cognitive performance, in order to assess their discriminant value, biological correlation, and diagnostic relevance.
The results show that blood p-tau181 and p-tau217 can effectively distinguish Alzheimer’s patients from controls, with diagnostic performance comparable to that of CSF (AUC > 0.88 in several studies). p-tau231 appears to be particularly sensitive to early changes, even preceding alterations detected by imaging. Moreover, plasma p-tau concentrations are correlated with cognitive decline, amyloid and tau brain burden, and the age of symptom onset. These markers are also able to differentiate Alzheimer’s from other neurodegenerative dementias (DLB, FTD), making them valuable for early differential diagnosis.
Alzheimer’s disease remains the leading cause of dementia, characterized by the accumulation of beta-amyloid and phosphorylated tau in the brain. Diagnosis still depends on invasive and poorly accessible examinations, hindering early detection and access to targeted care.
The aim of this review was to evaluate the potential of blood-based p-tau biomarkers (p-tau181, p-tau217, p-tau231) as non-invasive diagnostic tools. The results confirm their strong discriminant power, their correlation with central biomarkers, and their ability to identify Alzheimer’s from the earliest stages. These markers therefore pave the way for simpler, faster, and more equitable care, especially in primary care or large-scale contexts.
However, limitations remain and justify further research. It is essential to standardize assay methods, validate these markers in more diverse populations, and assess their feasibility in routine clinical practice. Integrating these data into algorithms that combine imaging, cognition, and genetics could accelerate the emergence of precision medicine in neurodegeneration.
About the author – Ana Espino
As a scientific writer, Ana is passionate about bridging the gap between research and real-world impact. With expertise in immunology, virology, oncology, and clinical studies, she makes complex science clear and accessible. Her mission: to accelerate knowledge sharing and empower evidence-based decisions through impactful communication.
#Alzheimer #Tau #Neurology
Alzheimer’s disease is a progressive neurodegenerative disorder, responsible for irreversible cognitive decline and loss of autonomy, associated with the abnormal accumulation of beta-amyloid and phosphorylated tau in the brain. It is the leading cause of dementia worldwide. Diagnosis still relies heavily on invasive and costly tools: cerebrospinal fluid (CSF) biomarkers, brain imaging (amyloid or tau PET), and complex clinical assessments, which are often difficult to access in everyday practice. These limitations hinder early screening and the implementation of targeted therapeutic strategies, particularly in the silent stages of the disease.
In this context, a major challenge lies in the identification and development of reliable peripheral biomarkers, capable of detecting Alzheimer’s from its earliest stages, distinguishing it from other causes of dementia, and being easily integrated into primary care.
This review was therefore conducted to explore the diagnostic potential of blood-based phosphorylated tau markers (p-tau181, p-tau217, p-tau231), by analyzing their accuracy, their correlation with central biomarkers, and their clinical applicability on a large scale.
Can plasma tau really make the distinction?
This review is based on a critical analysis of longitudinal and cross-sectional clinical studies, conducted on cohorts of patients with Alzheimer’s, individuals with mild cognitive impairment (MCI), and healthy controls. Plasma concentrations of phosphorylated tau (p-tau181, p-tau217, p-tau231) were systematically compared with CSF biomarkers, amyloid and tau PET imaging, and clinical cognitive performance, in order to assess their discriminant value, biological correlation, and diagnostic relevance.
The results show that blood p-tau181 and p-tau217 can effectively distinguish Alzheimer’s patients from controls, with diagnostic performance comparable to that of CSF (AUC > 0.88 in several studies). p-tau231 appears to be particularly sensitive to early changes, even preceding alterations detected by imaging. Moreover, plasma p-tau concentrations are correlated with cognitive decline, amyloid and tau brain burden, and the age of symptom onset. These markers are also able to differentiate Alzheimer’s from other neurodegenerative dementias (DLB, FTD), making them valuable for early differential diagnosis.
Towards a simple, rapid, and accessible diagnosis
Alzheimer’s disease remains the leading cause of dementia, characterized by the accumulation of beta-amyloid and phosphorylated tau in the brain. Diagnosis still depends on invasive and poorly accessible examinations, hindering early detection and access to targeted care.
The aim of this review was to evaluate the potential of blood-based p-tau biomarkers (p-tau181, p-tau217, p-tau231) as non-invasive diagnostic tools. The results confirm their strong discriminant power, their correlation with central biomarkers, and their ability to identify Alzheimer’s from the earliest stages. These markers therefore pave the way for simpler, faster, and more equitable care, especially in primary care or large-scale contexts.
However, limitations remain and justify further research. It is essential to standardize assay methods, validate these markers in more diverse populations, and assess their feasibility in routine clinical practice. Integrating these data into algorithms that combine imaging, cognition, and genetics could accelerate the emergence of precision medicine in neurodegeneration.
Read next: Single-cell epigenomic rewiring in alzheimer’s disease progression and cognitive resilience
About the author – Ana Espino
PhD in Immunology, specialized in Virology
Last press reviews
Turner syndrome and autoimmunity: an underestimated association?
By Ana Espino | Published on December 8, 2025 | 3 min read<br>
Could cinnamon become a natural treatment for metabolic syndrome?

By Lila Rouland | Published on December 5, 2025 | 3 min read<br><br>...
Who is afraid of Christmas? Do holidays trigger psychiatric crises?

By Carolina Lima | Published on Décember 4, 2025 | 3 min read