2025-11-20
Digital rectal exam in prostate cancer screening: time to rethink its role?
Oncology
By Carolina Lima | Published on November 20, 2025 | 3 min read
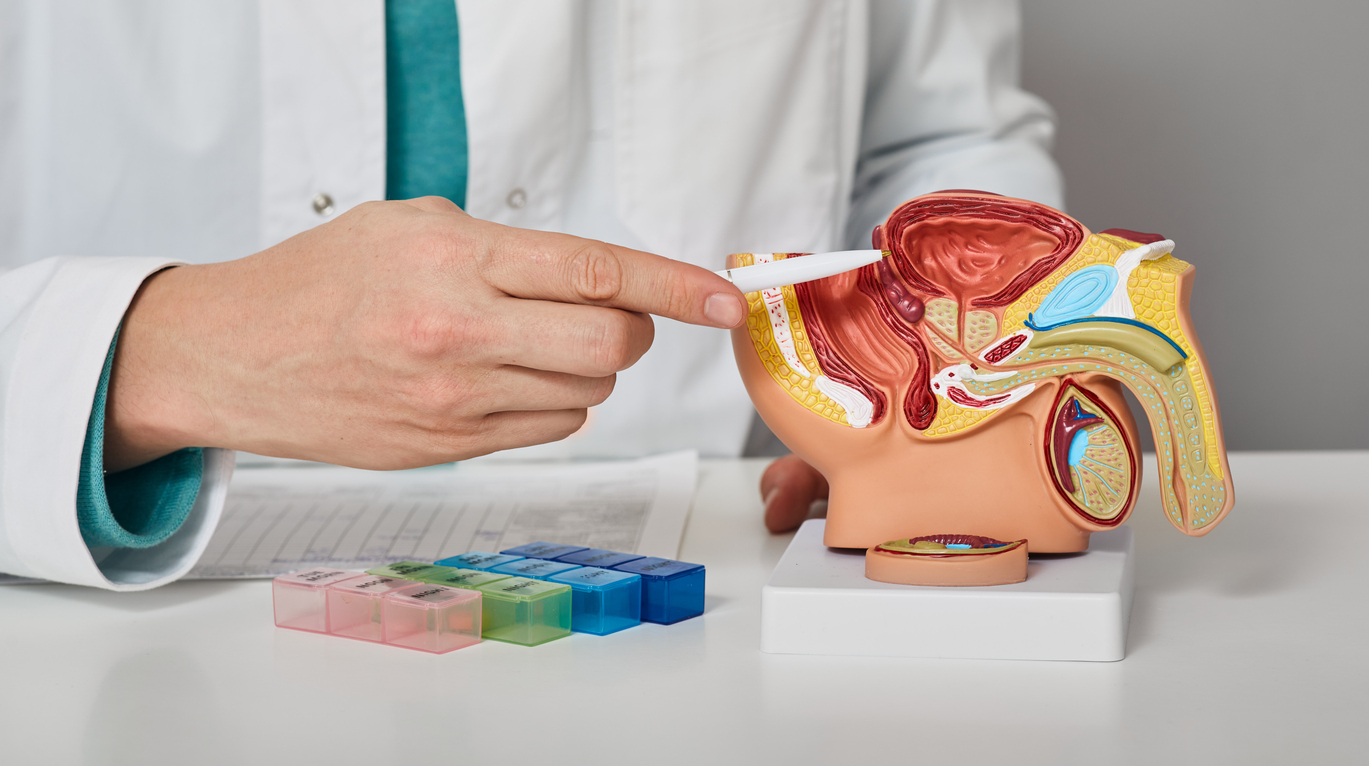
The digital rectal exam (DRE) has historically been a key tool in the early detection of prostate cancer (PCa). Before the widespread use of prostate-specific antigen (PSA) testing, DRE was the primary method for identifying potentially aggressive tumors. PSA transformed early detection by identifying cancers even in asymptomatic men, leading to a shift in screening practices. As PSA became standard, the value of DRE in routine screening has been increasingly questioned.
Despite this shift, some guidelines—like those from the French Urology Association (AFU)—still recommend combining DRE with PSA. This review revisits the evidence, focuses on findings from the European Randomized Study of Screening for Prostate Cancer (ERSPC), Rotterdam study, to assess whether DRE remains relevant in today’s screening protocols.
The ERSPC, one of the largest and most influential trials in prostate cancer screening, involved over 180,000 men across eight European countries. Its findings showed a 21% reduction in prostate cancer mortality in the PSA-screened group. DRE was initially included in screening protocols but was gradually discontinued. By the late 1990s, many centers had stopped performing DRE altogether, especially for men with PSA levels below 1 ng/mL.
The ERSPC investigators conducted several analyses to evaluate DRE’s utility. One early study found that DRE had a low positive predictive value, particularly in men with PSA levels under 4 ng/mL. In fact, hundreds of DREs were needed to detect a single clinically significant cancer in this group. Many of the tumors identified were small, low-grade, and likely false positives.
Several studies cited in the review highlight the limitations of DRE:
While some guidelines, like those from the French Urology Association (AFU), still recommend combining DRE with PSA, evidence shows limited added value. While DRE may help identify high-grade cancers when combined with elevated PSA levels, DRE rarely detects aggressive cancers on its own, especially in men with PSA between 2–3.9 ng/mL.
Later ERSPC findings confirmed PSA’s superiority: lowering the PSA threshold to 3 ng/mL and removing DRE improved accuracy and reduced unnecessary biopsies. By the third screening round, PSA alone accounted for 97–98% of cancer detections, with DRE contributing only 2–3%.
Large trials like The Göteborg (Sweden) and the CAP (UK) studies relied solely on PSA testing and confirmed its effectiveness in reducing prostate cancer mortality. In contrast, the PLCO trial (U.S.) included DRE but found no added survival benefit, suggesting DRE contributes little to PSA-based screening.
Some studies, like those by Borden et al., suggested that DRE might help identify high-grade cancers. However, these findings are mostly from diagnostic—not screening—and reproducibility remains a concern.
Evidence from ERSPC and others consistently shows that DRE adds little value to prostate cancer screening when PSA testing is available. While it may still have value in specific diagnostic scenarios, its routine use in screening is increasingly hard to justify. PSA testing offers greater accuracy, consistency, and patient comfort.
Future screening strategies should focus on personalized approaches using PSA levels and individual risk factors, minimizing unnecessary procedures. The review concludes that in regions with established PSA protocols, DRE no longer needs to be a standard part of screening.
About the Author – Carolina Lima
Carolina is a specialist in Anaesthesiology with a deep passion for learning and sharing medical knowledge. Dedicated to advancing the field, Dr. Lima strives to bring fresh, evidence-based insights to the medical community. Viewing medicine not merely as a profession but as a lifelong journey of continuous learning, Dr. Lima is committed to making complex information clear, practical, and useful for healthcare professionals around the world.
The digital rectal exam (DRE) has historically been a key tool in the early detection of prostate cancer (PCa). Before the widespread use of prostate-specific antigen (PSA) testing, DRE was the primary method for identifying potentially aggressive tumors. PSA transformed early detection by identifying cancers even in asymptomatic men, leading to a shift in screening practices. As PSA became standard, the value of DRE in routine screening has been increasingly questioned.
Despite this shift, some guidelines—like those from the French Urology Association (AFU)—still recommend combining DRE with PSA. This review revisits the evidence, focuses on findings from the European Randomized Study of Screening for Prostate Cancer (ERSPC), Rotterdam study, to assess whether DRE remains relevant in today’s screening protocols.
Insights from the ERSPC Study
The ERSPC, one of the largest and most influential trials in prostate cancer screening, involved over 180,000 men across eight European countries. Its findings showed a 21% reduction in prostate cancer mortality in the PSA-screened group. DRE was initially included in screening protocols but was gradually discontinued. By the late 1990s, many centers had stopped performing DRE altogether, especially for men with PSA levels below 1 ng/mL.
The ERSPC investigators conducted several analyses to evaluate DRE’s utility. One early study found that DRE had a low positive predictive value, particularly in men with PSA levels under 4 ng/mL. In fact, hundreds of DREs were needed to detect a single clinically significant cancer in this group. Many of the tumors identified were small, low-grade, and likely false positives.
Limitations of DRE
Several studies cited in the review highlight the limitations of DRE:
- Poor reproducibility: Results vary widely, even among experienced urologists.
- Limited value in low PSA levels: DRE failed to reliably detect significant cancers when PSA is below 4 ng/mL.
- Reduced screening participation: Up to 22% of men decline screening when DRE is included, due to discomfort or reluctance.
Selective use vs. routine screening
While some guidelines, like those from the French Urology Association (AFU), still recommend combining DRE with PSA, evidence shows limited added value. While DRE may help identify high-grade cancers when combined with elevated PSA levels, DRE rarely detects aggressive cancers on its own, especially in men with PSA between 2–3.9 ng/mL.
Later ERSPC findings confirmed PSA’s superiority: lowering the PSA threshold to 3 ng/mL and removing DRE improved accuracy and reduced unnecessary biopsies. By the third screening round, PSA alone accounted for 97–98% of cancer detections, with DRE contributing only 2–3%.
Global Trends
Large trials like The Göteborg (Sweden) and the CAP (UK) studies relied solely on PSA testing and confirmed its effectiveness in reducing prostate cancer mortality. In contrast, the PLCO trial (U.S.) included DRE but found no added survival benefit, suggesting DRE contributes little to PSA-based screening.
Some studies, like those by Borden et al., suggested that DRE might help identify high-grade cancers. However, these findings are mostly from diagnostic—not screening—and reproducibility remains a concern.
Conclusion: moving toward PSA-based screening
Evidence from ERSPC and others consistently shows that DRE adds little value to prostate cancer screening when PSA testing is available. While it may still have value in specific diagnostic scenarios, its routine use in screening is increasingly hard to justify. PSA testing offers greater accuracy, consistency, and patient comfort.
Future screening strategies should focus on personalized approaches using PSA levels and individual risk factors, minimizing unnecessary procedures. The review concludes that in regions with established PSA protocols, DRE no longer needs to be a standard part of screening.
Read next: Can the tumor transcriptomic profile predict immunotherapy efficacy?
About the Author – Carolina Lima
Anaesthesiology specialist
Carolina is a specialist in Anaesthesiology with a deep passion for learning and sharing medical knowledge. Dedicated to advancing the field, Dr. Lima strives to bring fresh, evidence-based insights to the medical community. Viewing medicine not merely as a profession but as a lifelong journey of continuous learning, Dr. Lima is committed to making complex information clear, practical, and useful for healthcare professionals around the world.
Last press reviews
Liver, sugar, and pills: who's in control?

By Ana Espino | Published on February 4, 2026 | 3 min read<br>
Endometrial cancer: Is PARP bringing new hope?
By Ana Espino | Published on February 3, 2026 | 3 min read<br>
