2025-05-26
Parkinson’s disease: could it all start in the gut?
Gastroenterology and Hepatology Neurology
#Parkinson #Microbiota #Dysbiosis
#Neurogastroenterology #GutHealth #Neuroinflammation
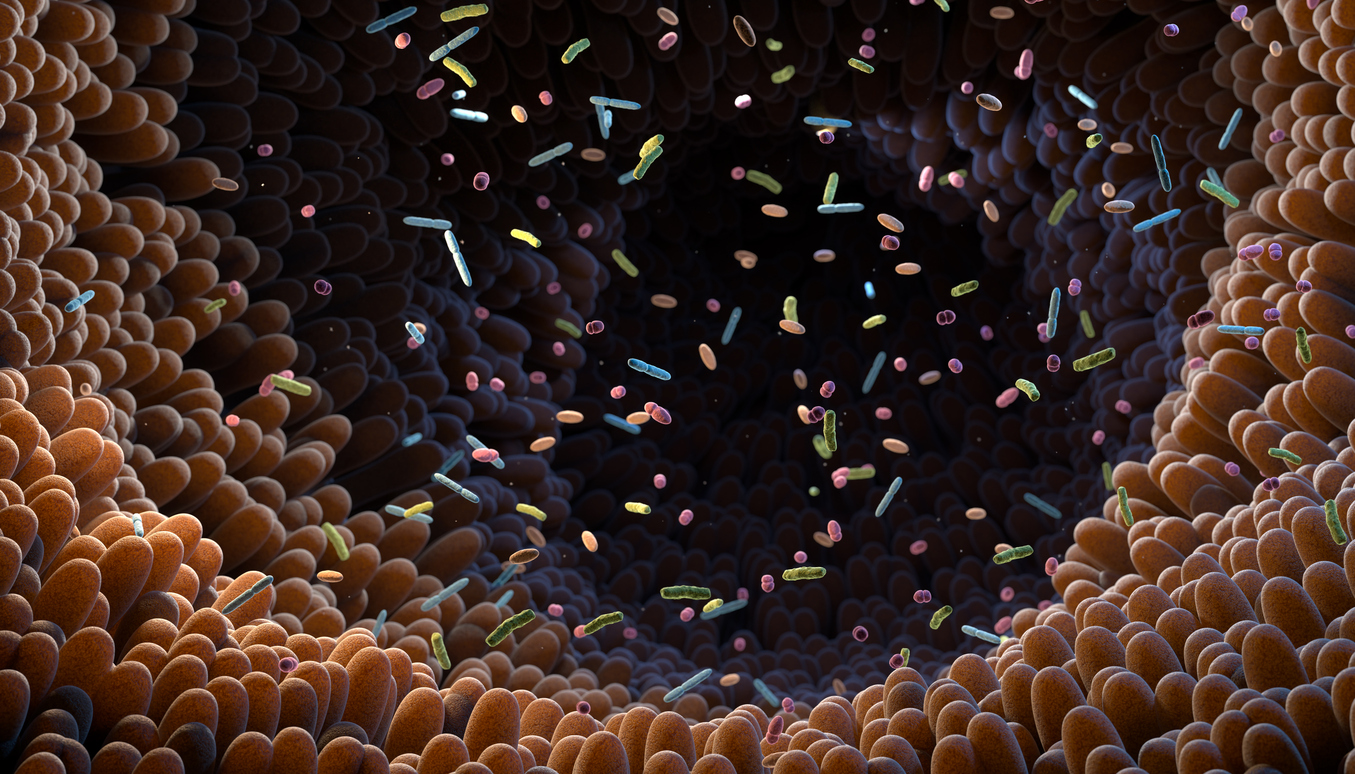
Parkinson’s disease (PD) is a progressive neurodegenerative disorder that affects approximately 1% of people over the age of 60. It manifests with motor symptoms such as resting tremors, muscle rigidity, bradykinesia (slowness of movement), and postural instability. However, non-motor symptoms such as constipation, sleep disturbances, mood changes, and cognitive issues suggest that more than just the central nervous system is involved. These observations have led to the hypothesis that Parkinson’s may originate in the gut.
In light of growing interest in this theory, numerous studies have investigated the relationship between the gut microbiota and Parkinson’s disease. The microbiota plays a key role in many physiological functions, including immune regulation, neurotransmitter production, intestinal permeability, and the synthesis of neuroprotective metabolites such as short-chain fatty acids (SCFAs) and polyamines. In Parkinson’s disease, alterations in microbiota composition could contribute to intestinal inflammation, increased epithelial barrier permeability, and the onset or progression of neurodegeneration. However, current results vary widely depending on the populations studied. This heterogeneity is attributed to geographic, dietary, genetic, and methodological factors, making it difficult to identify consistent and reproducible microbial signatures worldwide.
In this context, the present study was launched to shed light on the role of the gut microbiota in the pathogenesis of Parkinson’s disease and to identify targeted therapeutic avenues based on internationally shared microbial alterations.
In this study, fecal samples from Parkinson’s patients were compared with those of healthy controls. Shotgun metagenomic sequencing was used to characterize the bacterial and functional composition of the gut microbiota. Fecal concentrations of SCFAs and polyamines—two key metabolite families in gut and brain health—were also analyzed.
The analysis revealed significantly higher α-diversity in the microbiota of Parkinson’s patients, indicating greater richness and more even distribution of bacterial species. This increase in diversity suggests a profound reorganization of the gut microbiota in PD.
From a taxonomic perspective, notable changes were observed. Akkermansia muciniphila, a mucin-degrading bacterium, was significantly more abundant in patients, while Roseburia intestinalis and Faecalibacterium prausnitzii—both known butyrate producers—were markedly reduced. These findings point to dysbiosis characterized by a reduction in beneficial bacteria and a potential compromise of the intestinal mucosal barrier.
Functionally, there was a marked reduction in bacterial genes involved in the biosynthesis of riboflavin (vitamin B2) and biotin (vitamin B7). Additionally, five out of the six major families of carbohydrate-active enzymes responsible for dietary polysaccharide degradation were significantly reduced, suggesting an overall weakening of bacterial fiber metabolism.
Metabolically, fecal levels of SCFAs were clearly reduced in patients, as were levels of the polyamines putrescine, spermidine, and spermine. These molecules are essential for maintaining epithelial integrity, immune modulation, and neuroprotection.
Lastly, positive correlations were found between the abundance of bacterial genes for riboflavin and biotin biosynthesis and fecal levels of SCFAs and polyamines. This link suggests a shared metabolic signature characterized by functional loss of the microbiota in PD, directly connecting microbial deficits to biochemical alterations that may impact neuroinflammation and disease progression.
Parkinson’s disease is a complex neurodegenerative condition, and the role of the gut microbiota in its progression is increasingly acknowledged. One of the major challenges lies in the significant geographic variability of microbial composition and the heterogeneity of bacterial species responsible for functional alterations, complicating the identification of common targets. This study aimed to identify shared functional microbial alterations associated with disease-specific intestinal metabolic imbalances.
The results highlight a characteristic dysbiosis associated with reduced biosynthesis of riboflavin and biotin, along with decreased fecal SCFAs and polyamines—compounds essential for maintaining gut integrity and neuroimmune regulation. These findings suggest an active role of the microbiota in amplifying pathological processes in both the gut and the nervous system in Parkinson’s.
The data offer promising therapeutic perspectives. Supplementation with riboflavin and biotin could represent a targeted strategy to compensate for the functional deficits of the microbiota. Moreover, strengthening the intestinal barrier by modulating the microbiota may help slow the spread of α-synuclein aggregates and limit neurogenic inflammation—two central mechanisms in the progression of Parkinson’s disease.
Parkinson’s disease (PD) is a progressive neurodegenerative disorder that affects approximately 1% of people over the age of 60. It manifests with motor symptoms such as resting tremors, muscle rigidity, bradykinesia (slowness of movement), and postural instability. However, non-motor symptoms such as constipation, sleep disturbances, mood changes, and cognitive issues suggest that more than just the central nervous system is involved. These observations have led to the hypothesis that Parkinson’s may originate in the gut.
In light of growing interest in this theory, numerous studies have investigated the relationship between the gut microbiota and Parkinson’s disease. The microbiota plays a key role in many physiological functions, including immune regulation, neurotransmitter production, intestinal permeability, and the synthesis of neuroprotective metabolites such as short-chain fatty acids (SCFAs) and polyamines. In Parkinson’s disease, alterations in microbiota composition could contribute to intestinal inflammation, increased epithelial barrier permeability, and the onset or progression of neurodegeneration. However, current results vary widely depending on the populations studied. This heterogeneity is attributed to geographic, dietary, genetic, and methodological factors, making it difficult to identify consistent and reproducible microbial signatures worldwide.
In this context, the present study was launched to shed light on the role of the gut microbiota in the pathogenesis of Parkinson’s disease and to identify targeted therapeutic avenues based on internationally shared microbial alterations.
The microbiota: a silent accomplice in Parkinson’s?
In this study, fecal samples from Parkinson’s patients were compared with those of healthy controls. Shotgun metagenomic sequencing was used to characterize the bacterial and functional composition of the gut microbiota. Fecal concentrations of SCFAs and polyamines—two key metabolite families in gut and brain health—were also analyzed.
The analysis revealed significantly higher α-diversity in the microbiota of Parkinson’s patients, indicating greater richness and more even distribution of bacterial species. This increase in diversity suggests a profound reorganization of the gut microbiota in PD.
From a taxonomic perspective, notable changes were observed. Akkermansia muciniphila, a mucin-degrading bacterium, was significantly more abundant in patients, while Roseburia intestinalis and Faecalibacterium prausnitzii—both known butyrate producers—were markedly reduced. These findings point to dysbiosis characterized by a reduction in beneficial bacteria and a potential compromise of the intestinal mucosal barrier.
Functionally, there was a marked reduction in bacterial genes involved in the biosynthesis of riboflavin (vitamin B2) and biotin (vitamin B7). Additionally, five out of the six major families of carbohydrate-active enzymes responsible for dietary polysaccharide degradation were significantly reduced, suggesting an overall weakening of bacterial fiber metabolism.
Metabolically, fecal levels of SCFAs were clearly reduced in patients, as were levels of the polyamines putrescine, spermidine, and spermine. These molecules are essential for maintaining epithelial integrity, immune modulation, and neuroprotection.
Lastly, positive correlations were found between the abundance of bacterial genes for riboflavin and biotin biosynthesis and fecal levels of SCFAs and polyamines. This link suggests a shared metabolic signature characterized by functional loss of the microbiota in PD, directly connecting microbial deficits to biochemical alterations that may impact neuroinflammation and disease progression.
Read next: MoCA boosted, brain relieved!
A bacterial trail worth following?
Parkinson’s disease is a complex neurodegenerative condition, and the role of the gut microbiota in its progression is increasingly acknowledged. One of the major challenges lies in the significant geographic variability of microbial composition and the heterogeneity of bacterial species responsible for functional alterations, complicating the identification of common targets. This study aimed to identify shared functional microbial alterations associated with disease-specific intestinal metabolic imbalances.
The results highlight a characteristic dysbiosis associated with reduced biosynthesis of riboflavin and biotin, along with decreased fecal SCFAs and polyamines—compounds essential for maintaining gut integrity and neuroimmune regulation. These findings suggest an active role of the microbiota in amplifying pathological processes in both the gut and the nervous system in Parkinson’s.
The data offer promising therapeutic perspectives. Supplementation with riboflavin and biotin could represent a targeted strategy to compensate for the functional deficits of the microbiota. Moreover, strengthening the intestinal barrier by modulating the microbiota may help slow the spread of α-synuclein aggregates and limit neurogenic inflammation—two central mechanisms in the progression of Parkinson’s disease.
Read next: Can VR tip the balance?
Last press reviews
Colorectal cancer: a blood test to identify patients at risk of recurrence

By Ana Espino | Published on March 2nd, 2026 | 3 min read<br><br>
Cancer: when biotin becomes a therapeutic lever
By Elodie Vaz | Published on February 27, 2026 | 3 min read<br>
