2025-05-28
When the gut challenges MS
Allergology and Immunology Neurology
#MultipleSclerosis #Microbiota #Immunity
#Probiotics
Multiple sclerosis (MS) is an autoimmune neurological disorder characterized by chronic inflammation of the central nervous system (CNS) and the progressive destruction of the myelin sheath surrounding nerve fibers. This demyelination hinders the conduction of nerve impulses, leading to motor, sensory, cognitive, and visual impairments. While the exact origins of the disease remain incompletely understood, scientific consensus increasingly points to the key role of immune dysregulation. In particular, abnormal lymphocyte activation, excessive production of pro-inflammatory cytokines, and oxidative stress are recognized as key drivers of the inflammatory response that leads to neurological damage.
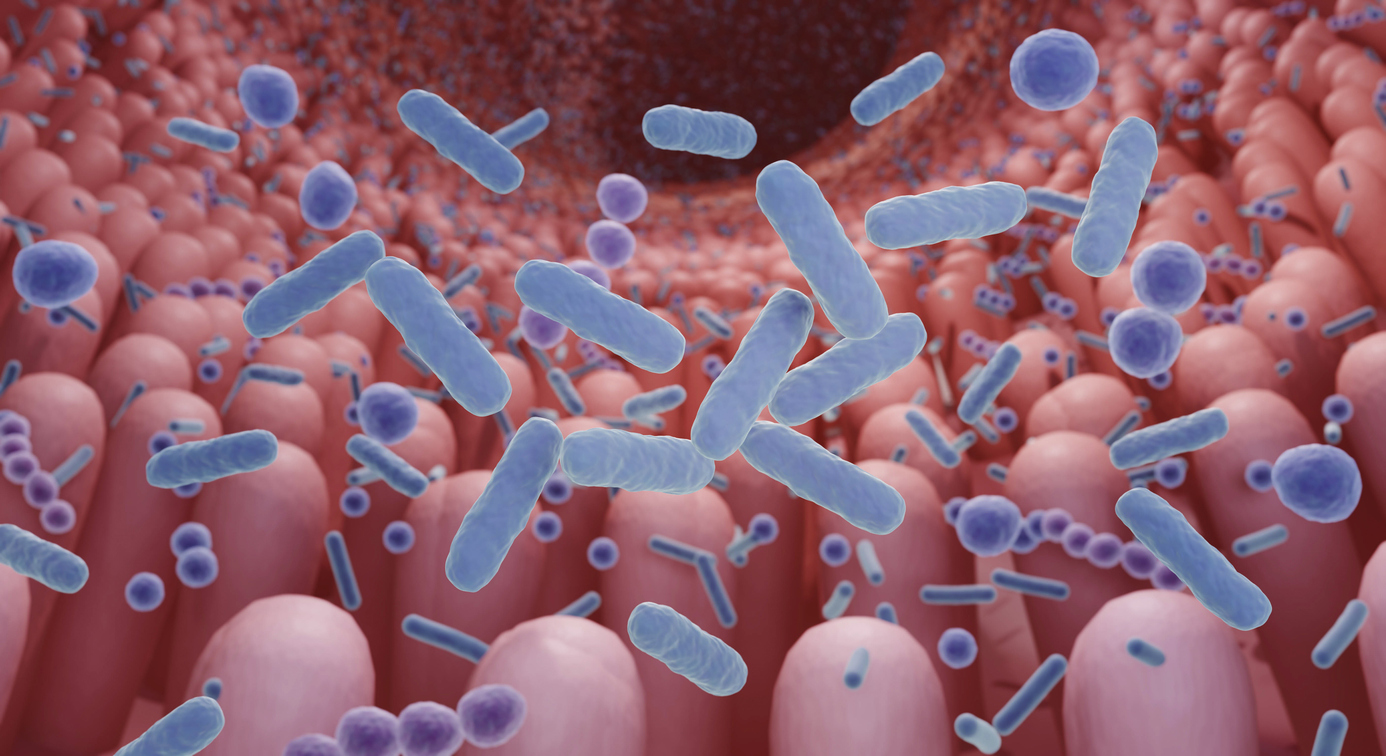
In recent years, a new line of research has emerged in the field of MS: the gut microbiota. This vast bacterial ecosystem is now acknowledged for its ability to continuously interact with the immune system and the brain via the “gut-brain axis.” Several experimental and clinical studies have revealed gut dysbiosis in MS patients, suggesting that microbiota imbalance may promote an inflammatory environment conducive to autoimmune activation.
It is in this context that probiotics come into play: live microorganisms—most often lactic acid bacteria—capable of restoring microbiota balance and favorably modulating the immune response. Proposed as an innovative therapeutic approach in chronic inflammatory diseases, they are generating increasing interest in neurology. This study aimed precisely to synthesize available data from both preclinical studies (animal models of MS) and clinical trials in humans to assess the actual potential of probiotics in modulating the progression of MS.
To comprehensively assess the effect of probiotics on multiple sclerosis, 23 studies were included in this analysis: 17 conducted on animal models (EAE) and 6 in human populations. The probiotics evaluated mainly included strains of Lactobacillus, Bifidobacterium, Prevotella, and Bacillus. Two groups were compared:
In animals, probiotics demonstrated strong immunomodulatory and anti-inflammatory effects. Their administration led to a marked decrease in pro-inflammatory cytokines such as interferon gamma, tumor necrosis factor alpha, and interleukin 17. At the same time, a significant increase in interleukin 10—a major anti-inflammatory cytokine—was observed in several studies. Clinically, treated animals showed significantly reduced symptom scores compared to control groups, indicating a reduction in disease severity. From an immunological standpoint, probiotics also helped restore the T-cell balance and increase the proportion of regulatory T cells (Tregs), known for their role in immune tolerance.
In humans, results pointed in the same direction. The trials showed a reduction in EDSS scores, an indicator of MS-related neurological disability progression. A decrease in pro-inflammatory cytokine levels was reported, along with favorable changes in gut microbiota composition. These findings suggest a potential effect of probiotics on the inflammatory environment and the gut-brain axis in patients with MS.
Multiple sclerosis is an autoimmune disease of the central nervous system marked by chronic inflammation and progressive demyelination, often resulting in severe neurological disabilities. One of the key mechanisms of the disease is immune system dysregulation, notably an overactivation of Th1 and Th17 lymphocytes. By targeting this imbalance, probiotics—through their ability to modulate immunity and restore microbiota composition—may offer a complementary, natural, and non-invasive therapeutic strategy in the treatment of MS.
This is precisely what the study aimed to explore: to assess the potential effectiveness of probiotics in reducing the progression of MS. The results are promising, especially in animals, where probiotics reduced inflammation, improved clinical parameters, and promoted activation of regulatory T cells. In humans, preliminary data suggest beneficial effects on inflammatory markers and clinical severity.
Although probiotics represent a major avenue for modulating immunity in MS patients, their actual efficacy has yet to be confirmed. Larger, standardized clinical studies are still needed to validate their role in therapeutic management.
Multiple sclerosis (MS) is an autoimmune neurological disorder characterized by chronic inflammation of the central nervous system (CNS) and the progressive destruction of the myelin sheath surrounding nerve fibers. This demyelination hinders the conduction of nerve impulses, leading to motor, sensory, cognitive, and visual impairments. While the exact origins of the disease remain incompletely understood, scientific consensus increasingly points to the key role of immune dysregulation. In particular, abnormal lymphocyte activation, excessive production of pro-inflammatory cytokines, and oxidative stress are recognized as key drivers of the inflammatory response that leads to neurological damage.
In recent years, a new line of research has emerged in the field of MS: the gut microbiota. This vast bacterial ecosystem is now acknowledged for its ability to continuously interact with the immune system and the brain via the “gut-brain axis.” Several experimental and clinical studies have revealed gut dysbiosis in MS patients, suggesting that microbiota imbalance may promote an inflammatory environment conducive to autoimmune activation.
It is in this context that probiotics come into play: live microorganisms—most often lactic acid bacteria—capable of restoring microbiota balance and favorably modulating the immune response. Proposed as an innovative therapeutic approach in chronic inflammatory diseases, they are generating increasing interest in neurology. This study aimed precisely to synthesize available data from both preclinical studies (animal models of MS) and clinical trials in humans to assess the actual potential of probiotics in modulating the progression of MS.
Microbiota to the rescue?
To comprehensively assess the effect of probiotics on multiple sclerosis, 23 studies were included in this analysis: 17 conducted on animal models (EAE) and 6 in human populations. The probiotics evaluated mainly included strains of Lactobacillus, Bifidobacterium, Prevotella, and Bacillus. Two groups were compared:
- Probiotic group: participants (animals or humans) received probiotics such as Lactobacillus or Bifidobacterium for several weeks.
- Control group: this group received no probiotics (placebo or no treatment).
In animals, probiotics demonstrated strong immunomodulatory and anti-inflammatory effects. Their administration led to a marked decrease in pro-inflammatory cytokines such as interferon gamma, tumor necrosis factor alpha, and interleukin 17. At the same time, a significant increase in interleukin 10—a major anti-inflammatory cytokine—was observed in several studies. Clinically, treated animals showed significantly reduced symptom scores compared to control groups, indicating a reduction in disease severity. From an immunological standpoint, probiotics also helped restore the T-cell balance and increase the proportion of regulatory T cells (Tregs), known for their role in immune tolerance.
In humans, results pointed in the same direction. The trials showed a reduction in EDSS scores, an indicator of MS-related neurological disability progression. A decrease in pro-inflammatory cytokine levels was reported, along with favorable changes in gut microbiota composition. These findings suggest a potential effect of probiotics on the inflammatory environment and the gut-brain axis in patients with MS.
Bacteria full of promise
Multiple sclerosis is an autoimmune disease of the central nervous system marked by chronic inflammation and progressive demyelination, often resulting in severe neurological disabilities. One of the key mechanisms of the disease is immune system dysregulation, notably an overactivation of Th1 and Th17 lymphocytes. By targeting this imbalance, probiotics—through their ability to modulate immunity and restore microbiota composition—may offer a complementary, natural, and non-invasive therapeutic strategy in the treatment of MS.
This is precisely what the study aimed to explore: to assess the potential effectiveness of probiotics in reducing the progression of MS. The results are promising, especially in animals, where probiotics reduced inflammation, improved clinical parameters, and promoted activation of regulatory T cells. In humans, preliminary data suggest beneficial effects on inflammatory markers and clinical severity.
Although probiotics represent a major avenue for modulating immunity in MS patients, their actual efficacy has yet to be confirmed. Larger, standardized clinical studies are still needed to validate their role in therapeutic management.
Read next: Ibudilast in multiple sclerosis
Last press reviews
Colorectal cancer: a blood test to identify patients at risk of recurrence

By Ana Espino | Published on March 2nd, 2026 | 3 min read<br><br>
Cancer: when biotin becomes a therapeutic lever
By Elodie Vaz | Published on February 27, 2026 | 3 min read<br>
