2025-07-23
Reprogramming fat to starve the tumor?
Oncology
By Lila Rouland | Published on July 23, 2025 | 3 min read
#Cancer #Adipocytes #TumorMetabolism #InnovativeTherapy
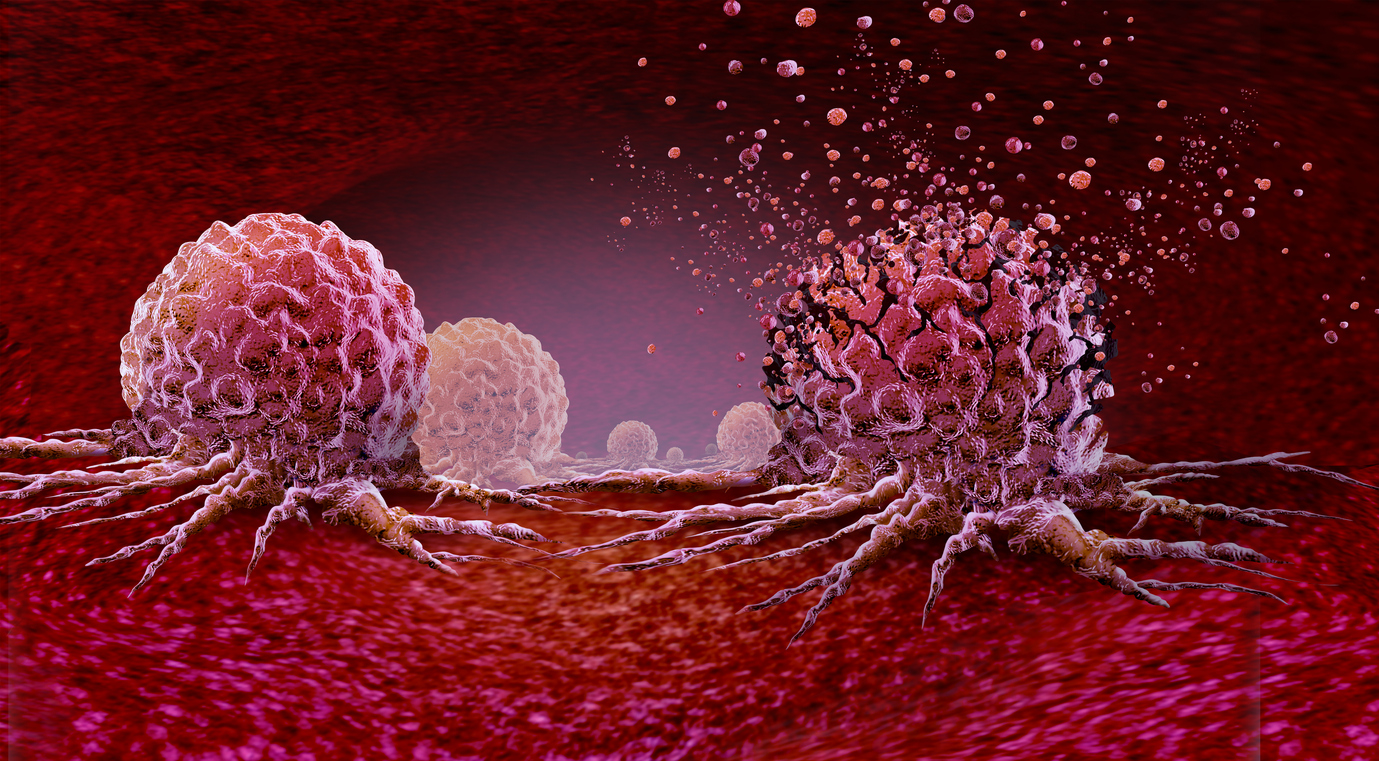
Cancer cells thrive in a microenvironment that is poor in oxygen and nutrients. To survive, they reprogram their metabolism to more efficiently absorb glucose (aerobic glycolysis, or the Warburg effect) and fatty acids (fatty acid oxidation, or FAO), enabling rapid proliferation.
In a groundbreaking strategy, researchers propose the transplantation of engineered adipose tissue (Adipose Manipulated Tissue, or AMT) to create “metabolic competition” within the tumor microenvironment. The goal? Force adipocytes to consume glucose and lipids so rapidly that the tumor can no longer access them. The results, published in Nature Biotechnology, are striking.
In this study, human adipocytes were genetically reprogrammed using CRISPRa technology to activate key genes of brown fat (UCP1, PRDM16, PPARGC1A), known for its high energy expenditure.
The result? These cells demonstrated a dramatic increase in oxygen, glucose, and fatty acid consumption—essentially switching into “turbo” metabolic mode. When injected near tumors in mice, the effect was radical: reduced tumor growth, lower glucose uptake, decreased blood vessel formation, and even signs of apoptosis.
Initially, these “brown-like” adipocytes were co-cultured with five human cancer cell lines (breast, colon, pancreas, prostate). Within three days:
CRISPRa adipocytes, especially those expressing UCP1, outperformed conventional metabolic treatments such as 6-aminonicotinamide (glycolysis inhibitor) and etomoxir (FAO inhibitor).
In mice, the implantation of modified adipose organoids adjacent to tumor xenografts led to a >50% reduction in tumor volume within 3 weeks. Treated tumors showed:
Analyses also showed a global depletion of glucose and lipids in tumors, as if the cancer cells could no longer feed themselves.
The UCP1-CRISPRa adipose organoids displayed:
When the mice were fed high-fat or high-sugar diets, the anti-tumor effect of CRISPRa adipocytes disappeared—confirming the crucial role of nutrient competition.
Transcriptomic (RNA-seq) analysis of tumors treated with CRISPRa adipocytes (under a normal diet) revealed:
The findings were validated in two established murine cancer models:
In both, CRISPRa adipose organoid implantation reduced tumor mass—regardless of implant location—with sustained effects and no weight loss or toxicity.
The researchers went a step further by using human adipocytes isolated from breast tissue. These were reprogrammed with UCP1-CRISPRa and co-cultured with patient-derived tumor organoids (triple-negative and HR+ breast cancers). Results:
This study shows that genetically modified human adipocytes can slow tumor progression by depriving cancer cells of essential nutrients. The approach:
Future work aims to validate this approach in humans and explore its application in other cancer types and metabolic targets.
About the Author – Lila Rouland
Doctor of Oncology, specialized in Biotechnology and Marketing
With dual expertise in science and marketing, Lila brings her knowledge to the service of healthcare innovation. After five years in international academic research, she transitioned into medical and scientific communication within the pharmaceutical industry. Now working as a medical writer and content developer, she is committed to highlighting scientific knowledge and conveying it to healthcare professionals with clarity and relevance.
#Cancer #Adipocytes #TumorMetabolism #InnovativeTherapy
Cancer cells thrive in a microenvironment that is poor in oxygen and nutrients. To survive, they reprogram their metabolism to more efficiently absorb glucose (aerobic glycolysis, or the Warburg effect) and fatty acids (fatty acid oxidation, or FAO), enabling rapid proliferation.
In a groundbreaking strategy, researchers propose the transplantation of engineered adipose tissue (Adipose Manipulated Tissue, or AMT) to create “metabolic competition” within the tumor microenvironment. The goal? Force adipocytes to consume glucose and lipids so rapidly that the tumor can no longer access them. The results, published in Nature Biotechnology, are striking.
Turning adipocytes into energy burners
In this study, human adipocytes were genetically reprogrammed using CRISPRa technology to activate key genes of brown fat (UCP1, PRDM16, PPARGC1A), known for its high energy expenditure.
The result? These cells demonstrated a dramatic increase in oxygen, glucose, and fatty acid consumption—essentially switching into “turbo” metabolic mode. When injected near tumors in mice, the effect was radical: reduced tumor growth, lower glucose uptake, decreased blood vessel formation, and even signs of apoptosis.
In vitro: tumor cell proliferation drops sharply
Initially, these “brown-like” adipocytes were co-cultured with five human cancer cell lines (breast, colon, pancreas, prostate). Within three days:
- A 3- to 5-fold reduction in tumor cell count.
- A decrease in MKI67 expression, a marker of proliferation.
- A drop in glycolysis (ECAR, GLUT4, GCK) and FAO (OCR, CD36, CPT1B).
CRISPRa adipocytes, especially those expressing UCP1, outperformed conventional metabolic treatments such as 6-aminonicotinamide (glycolysis inhibitor) and etomoxir (FAO inhibitor).
In vivo: tumors shrunk by half
In mice, the implantation of modified adipose organoids adjacent to tumor xenografts led to a >50% reduction in tumor volume within 3 weeks. Treated tumors showed:
- Lower levels of hypoxia (CA9),
- Reduced angiogenesis (CD31),
- Increased caspase-3, a marker of apoptosis.
Analyses also showed a global depletion of glucose and lipids in tumors, as if the cancer cells could no longer feed themselves.
A mechanism based on nutrient competition
The UCP1-CRISPRa adipose organoids displayed:
- High intracellular levels of glucose and fatty acids,
- While the associated tumors were depleted of glucose and glycolytic metabolites (G6P, F6P, etc.).
When the mice were fed high-fat or high-sugar diets, the anti-tumor effect of CRISPRa adipocytes disappeared—confirming the crucial role of nutrient competition.
Transcriptomic (RNA-seq) analysis of tumors treated with CRISPRa adipocytes (under a normal diet) revealed:
- 7,102 differentially expressed genes, including:
- 6,623 downregulated (e.g., MKI67, FASN, SCD, CPT1B),
- 479 upregulated (e.g., HOXD10, GAS7),
- Suppressed pathways related to cell growth, FAO, and cell division,
- Activated pathways linked to
apoptosis and cellular stress.
The effect was systemic and profound.
Effective in Genetic Cancer Models Too
The findings were validated in two established murine cancer models:
- The KPC pancreatic cancer model,
- The MMTV-PyMT breast cancer model.
In both, CRISPRa adipose organoid implantation reduced tumor mass—regardless of implant location—with sustained effects and no weight loss or toxicity.
What about humans? Promising results with breast tissue
The researchers went a step further by using human adipocytes isolated from breast tissue. These were reprogrammed with UCP1-CRISPRa and co-cultured with patient-derived tumor organoids (triple-negative and HR+ breast cancers). Results:
- Significant reduction in tumor organoid size and number,
- Decreased expression of MKI67, GLUT4, GCK, CD36, and CPT1B,
- Effects observed across five distinct clinical samples.
A new metabolic weapon against cancer
This study shows that genetically modified human adipocytes can slow tumor progression by depriving cancer cells of essential nutrients. The approach:
- Can be personalized (e.g., UPP1 activation to target uridine-dependent cancers),
- Uses autologous cells (from the patient),
- Is potentially reversible and remotely controllable (via tetracycline or biomaterial platforms).
Future work aims to validate this approach in humans and explore its application in other cancer types and metabolic targets.
Read next: Lipids and breast cancer: metabolic reprogramming as a therapeutic target
About the Author – Lila Rouland
Doctor of Oncology, specialized in Biotechnology and Marketing
With dual expertise in science and marketing, Lila brings her knowledge to the service of healthcare innovation. After five years in international academic research, she transitioned into medical and scientific communication within the pharmaceutical industry. Now working as a medical writer and content developer, she is committed to highlighting scientific knowledge and conveying it to healthcare professionals with clarity and relevance.
Last press reviews
Parental alcohol intoxication: the hidden impact on children’s mental health

By Carolina Lima | Published on January 19, 2026 | 3 min read
Obesity: when the kidneys become overwhelmed

By Ana Espino | Published on January 16, 2026 | 3 min read...
